Hemodynamics, Transport
2024 Q4 Critical Care Transport Update Webinar
In this Q4 critical care transport update webinar, Jena Billig, BSN, RN, CCRN, CFRCN, Abiomed’s West coast critical care transport trainer, discusses pulmonary artery catheters and why hemodynamic monitoring is important in patients supported with Impella.
Jena explains that pulmonary artery catheters (PACs)—also know as Swan-Ganz catheters or right heart catheters—provide real-time hemodynamic measures of how efficiently the heart is functioning. While PAC use has waxed and waned over the years as a result of various published data, Jena explains that recent data from Hernandez et al. demonstrates “the use of pulmonary artery catheters in patients with cardiogenic shock was shown to actually improve mortality and lower their rates of in-hospital cardiac arrest.”
Jena explains how PACs can be used to monitor right atrial (RA) or central venous pressure (CVP), right ventricular systolic and diastolic pressures, pulmonary artery systolic and diastolic pressures and venous oxygen saturation (SVO2). They can directly measure pulmonary capillary wedge pressure (PCWP) and cardiac output (CO) and provide indirect measures of left atrial pressure (LAP) and left ventricular end diastolic pressure (LVEDP). Other hemodynamic values, such as pulmonary vascular resistance (PVR), pulmonary artery pulsatility index (PAPi), cardiac index (CI), systemic vascular resistance (SVR) and cardiac power output (CPO), can be calculated.
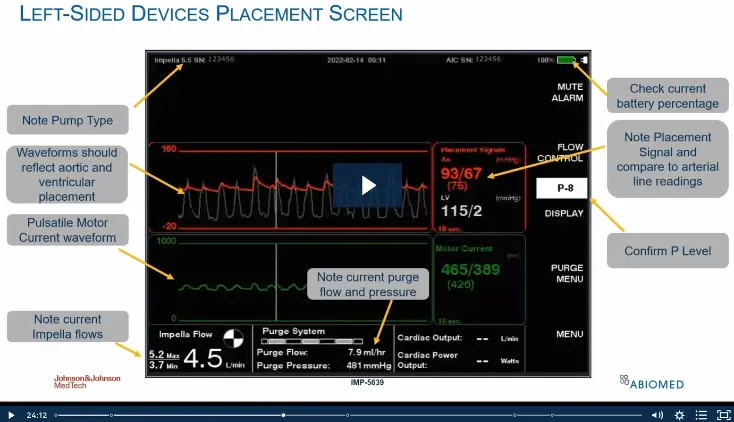
The Preload-Afterload-Positioning (P-A-P) mnemonic provides a memorable way to think about Impella patient management during transport. Jena explains that Impella is preload dependent and there must be volume in order to move volume with Impella. She also explains that Impella is afterload sensitive and that correct positioning is critical for optimal Impella function and patient outcomes. She reviews how to determine whether there is good P-A-P and how to maintain proper preload, afterload, and position.
Jena then focuses on how Impella improves hemodynamics. She explains that it increases mean arterial pressure (MAP), CO, and cardiac power output (CPO), and reduces PCWP. She discusses how CPO and lactate levels can predict survival at 12-24 hours on Impella. She also explains how invasive hemodynamic measurement with PAPi may identify patients with severe right ventricular dysfunction while predicting in-hospital mortality risk and the need for mechanical circulatory support (MCS) or escalation of MCS.
NPS-5128