
Early Identification of AMICS Patient’s Level of Shock is Critical to a Positive Outcome1,2
The paper "Treatment Intensity for the Management of Cardiogenic Shock: Comparison between STEMI and Non-STEMI" by Shashank S. Sinha, MD, MSC, and colleagues examines clinical characteristics, mortality, and device usage in 1,110 patients with acute myocardial infarction cardiogenic shock (AMI-CS). Mortality rates were similar between patients with STEMI-CS (43%) and NSTEMI-CS (39%).
The study demonstrated that the majority of SCAI stage B and C patients progressed to SCAI stages D and E during their hospitalization and patients transitioning to a higher SCAI stage had worse in-hospital outcomes compared to patients who initially presented in SCAI stage E. Patients with out-of-hospital cardiac arrest (OHCA) or in-hospital-cardiac arrest (IHCA) also had higher in-hospital mortality. While only 27% of patients with STEMI-CS and 12% of patients with NSTEMI-CS received both a drug and tMCS during the first 24 hours, drug and device use increased throughout hospitalization in all patients.
The authors conclude, “Despite increasing use of inotropic and vasoactive support and tMCS throughout the course of the hospitalization, both patients with STEMI-CS and NSTEMI-CS remain at increased risk for in-hospital mortality. Future RCTs are needed to elucidate whether timing and sequence of escalation of support improves outcomes in these critically ill patients.”
Why is Stage B for Bad
Decoding Cardiogenic Shock: SCAI and CSWG's Breakdown of Shock Stages
This following graphic illustrates the Society for Cardiovascular Angiography and Intervention (SCAI) shock stages as well as the Cardiogenic Shock Working Group (CSWG) interpretation of the SCAI shock stages.
Note that SCAI-CSWG stage B is defined as hypotensive or hypoperfusing and untreated, and SCAI-CSWG stage C is defined as patients who are hypotensive and hypoperfusing or patients who are treated for CS with 1 drug or 1 circulatory support device.
Early Identification of Cardiogenic Shock Improves Outcomes
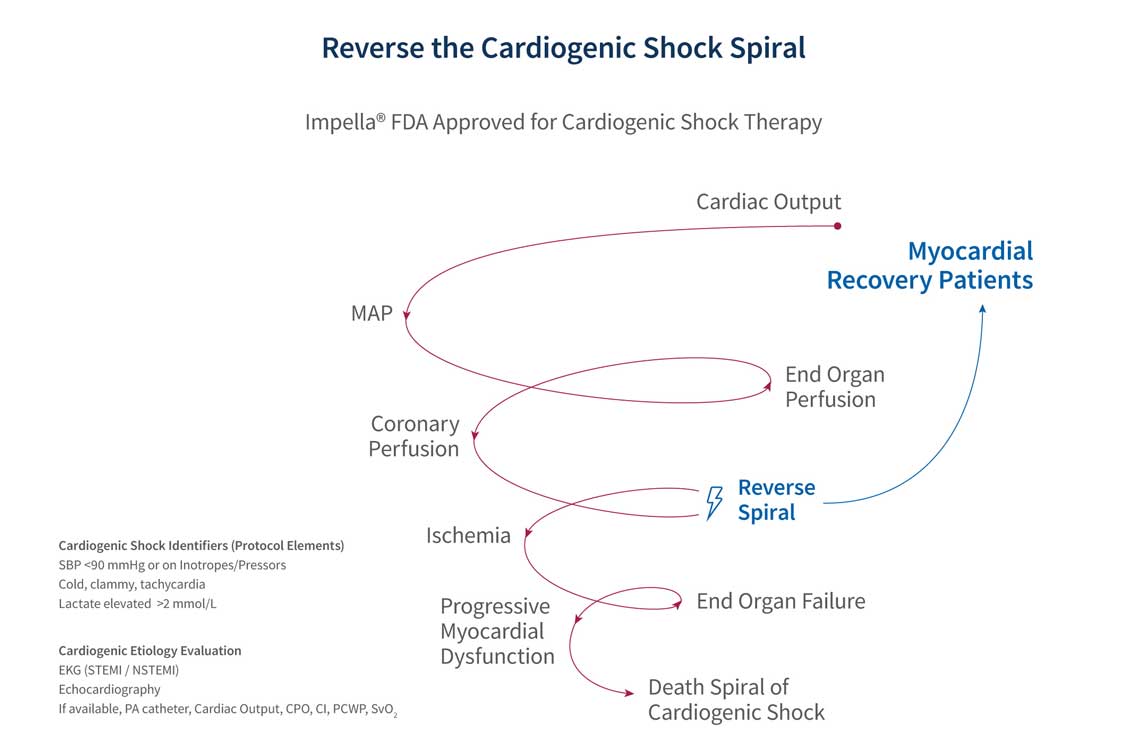
Timely treatment adhering to a best practice protocol, that includes early use of mechanical circulatory support, hemodynamic monitoring, and aggressive reduction of inotropes and pressors, can help patients achieve myocardial recovery.3
Discover Additional Resources about Patient Identification in Cardiogenic Shock
References
- Kapur NK, et al. 2022. J Am Coll Cardiol. 80 (3):185-198, https://doi.org/10.1016/j.jacc.2022.04.049
- Hanson ID, et al. 2024. J Am Heart Assoc. 13(3):e031803. doi:10.1161/JAHA.123.031803.
- O'Neill, W.W., TCT 2020.
NPS-4723







